Allergic Rhinitis Diagnosis
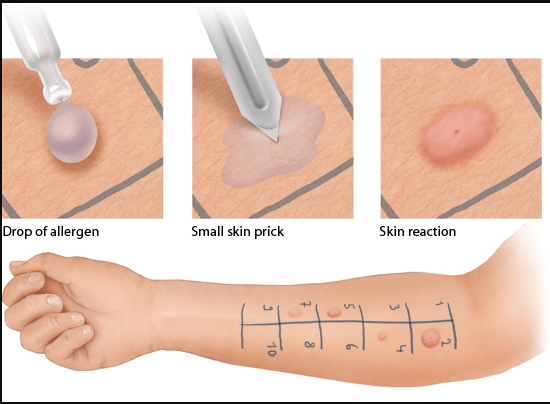
The diagnosis of allergic rhinitis (AR, nose inflammation caused by allergies) is made by the patient’s medical history, a physical examination, and if needed, nasal endoscopy. In addition, some patients may be tested for allergen-specific IgE using skin prick tests or tests for serum-specific IgE. A skin prick test is when distinct allergens are pricked into the skin to measure the inflammation reaction. A blood test quantifies allergen-specific IgE titer. These tests are used to identify or confirm specific allergens; testing can support the diagnosis and is mandatory when allergy immunotherapy (AIT) is being considered. The results of IgE testing may produce false positives and negatives and need to be professionally interpreted because IgE titer does not necessarily correspond to symptomatic allergy.
Some additional tests that may be done are nasal allergen provocation tests–which can be used when the medical history and systemic IgE results are not consistent–nasal cytology, and ciliary beat frequency analysis. Additionally, in some centers, nasal smear cytology is practiced.
The presence of a high number of eosinophils suggests an inflammatory process but not necessarily AR. Unilateral eosinophilia can occur, so bilateral samples must be taken from the nostrils. Nasal nitric oxide measurement is a rapid test that discriminates AR, non-allergic rhinitis, and other inflammations of the nose such as sinusitis, nasal polyps, and middle ear infections; this can only be done in highly specialized centers.
Currently, there are few novel drug candidates for AR because of the general success of over-the-counter mediation in alleviating the symptoms of AR in most cases.
Desensitization
Desensitization is a common long-term allergy cure for individuals with multiple allergies, also known as Allergy Immunotherapy (AIT). This treatment is a safe way to train your body to tolerate the allergens and irritants causing your allergic responses. This process uses gradual exposure and has many different options for getting the allergen into your body. The overall success rate varies depending on what method you use, the kinds of allergies you have, and the severity of those allergies; however, the success rate is fairly high for all forms of desensitization (around 80%) and can even decrease hereditary allergies as much as up to 56%.
Desensitization helps most forms of allergies and has even been approved for food allergens that are more likely to cause anaphylactic shock, such as nuts, milk, eggs, shellfish, and wheat. Some other allergens that are amenable to desensitization are environmental (such as dust mites), animal (cat and dog dander), and natural allergens (mold, grass, trees, dust, etc.)
One option for desensitization is oral immunotherapy (OIT), used for food allergies. There are two phases in this process. In the first phase, tiny amounts of the problem food in a solution will be introduced. Then, gradually, the dosage of the allergen will increase (more concentrated solution). Then when it is safe, you will get small amounts of the whole food. Eventually, most people who chose this treatment can safely consume foods that they were allergic to. The timing for this form of desensitization depends on the severity of the allergy and whether or not you can be at risk of an anaphylactic reaction.
Another option is subcutaneous immunotherapy, where injections are used to achieve allergy desensitization. A tiny amount of the allergen will be injected at intervals, gradually increasing the potency. At the end of the treatment, most patients no longer suffer from their symptoms. The timing for this takes about three to five years, most commonly consisting of a shot once a week for a year and then once every two weeks the next year and continuing until just the maintenance shot once a year.
A different option is sublingual immunotherapy, where drops that dissolve under the tongue are used. They are convenient because you generally don’t have to come to your allergist’s office for many separate appointments throughout your treatment. The allergens that have been approved by the FDA for this method are ragweed, timothy grass, dust mites, and a combination of five grass species.
Atopic Dermatitis Diagnosis
The atopy patch test can identify allergens for atopic dermatitis (AD), also known as atopic eczema. In an atopy patch test, the whole fresh allergen is applied to the skin and covered (by medical tape or another method) to prevent any other things from getting into the test sites. The patch test is typically performed over three days. Then the inflammatory reactions are measured to determine the allergy and the severity of the allergy. Atopic dermatitis severity can be measured using scoring systems such as the Scoring Atopic Dermatitis (SCORAD) or Eczema Area and Severity Index (EASI).

Atopic Dermatitis Treatments
In moderate forms, AD/AE should be treated early and aggressively with topical steroids (Mometasone, Clobetasol propionate) and when in remission with a pro‐active therapy. Severe forms of AD/AE might be treated with the systemic immunosuppressants cyclosporine, methotrexate, azathioprine, or mycophenolate mofetil. However, all of these therapies are of limited effectiveness and have long‐term side effects. The use of strong steroids can cause fluid retention in the legs, high blood pressure, bone damage through thinning, Cushing syndrome, and in children can affect growth. Immunosuppressants can cause an increased risk of infections, upset stomach and vomiting, increased risk for certain types of cancers, increased blood pressure with cyclosporine, Increased risk of kidney damage with cyclosporine and methotrexate, and risk of liver damage with methotrexate.
Biologics are currently being researched for AD/AE. Biologics have been approved for other skin diseases such as psoriasis, most of them targeting non-type two pathways such as type 3 (Th17) immunity or the cytokines IL‐6 or IL‐1b to dampen acute phase reactions or to neutralize type 2 (Th2) immunity. Biologics that have been highly efficient for psoriasis have failed to prove efficacy in AE. Dupilumab was approved for moderate to severe AE in the US and Europe in 2017 (see more below in asthma section).
Allergic Asthma Diagnosis
Your doctor will look at your medical history to see if asthma or allergy is common in your family or if you are more likely to have asthma because of other irritants. Additionally, your doctor will perform a physical examination where they may examine your nose, throat, and airways. They may also listen for wheezing in your breathing or check if you have any allergic conditions like AE/ AD or hives.
The primary diagnostic test for people over five years old is performed using a spirometer. Spirometry checks your pulmonary function; you take a deep breath and exhale forcefully into a tube connected to a spirometer. This records both the volume of air and how quickly you exhaled. If specific measurements are below average for a person your age, it may indicate that asthma has narrowed your airways. If your spirometry results come out normal and you appear to have exercise-induced asthma, you may be asked to do physical activity and retake the spirometry test. You may also take a nitric oxide test where you will breathe into a tube that measures the amount of nitric oxide gas in your breath. High levels in your breath may mean you have inflamed airways, a sign of asthma.
Your doctor may run additional tests if they suspect you may have a condition other than asthma, such as x-rays or CT scans of your chest or sinuses, blood tests, gastroesophageal reflux assessment, or an examination of the phlegm in your lungs to see if it may be a viral or bacterial infection.
Doctors rarely do lung tests on children under five. Instead, these children are typically diagnosed based on their medical history, signs and symptoms, and a physical examination. It is difficult to diagnosis a child in this age group with asthma because of the number of conditions that cause asthma-like symptoms in this age group.
Asthma Treatments
It is very common to be prescribed an inhaler if you have asthma. Inhalers (inhaled corticosteroids) are the most effective and commonly used anti-inflammatory drug for asthma as they reduce swelling and tightening in the airways. Please note that you may need to use these medications for several months before you get their maximum benefit. Some examples are Fluticasone (Flovent HFA), Budesonide (Pulmicort Flexhaler), Mometasone (Asmanex Twisthaler), Beclomethasone (Qvar RediHaler), and Ciclesonide (Alvesco). Regular use of inhaled corticosteroids helps keep asthma attacks and other symptoms in check. Side effects are uncommon but tend to be
mouth irritation, throat irritation, and oral yeast infections. Some other inhalers combine corticosteroids and long-acting beta-agonists like Fluticasone and salmeterol (Advair Diskus), Budesonide and formoterol (Symbicort), Mometasone and formoterol (Dulera), and Fluticasone and vilanterol (Breo).
The current targets for biologic therapy for type 2 asthma are IgE (Omalizumab), IL‐5 (mepolizumab and Reslizumab), IL‐5Ra (benralizumab), and IL‐4Ra (dupilumab).
Omalizumab is a humanized, monoclonal antibody that binds and neutralizes IgE. It is used on patients with moderate to severe allergic asthma that are older than six years old. Omalizumab prevents IgE from binding to its high‐affinity receptor (FcεRI) on mast cells and basophils, blocking their allergic response and downregulates the expression of high‐affinity IgE receptors on mast cells. As a result, Omalizumab reduces asthma exacerbation (by ~25%), reduces hospital admissions, and also specifically decreases virus‐associated exacerbations, possibly by increasing anti‐viral response from dendritic cells. Omalizumab is well tolerated and has a low risk of anaphylaxis.
Benralizumab is directed against IL‐5Ra, which is highly expressed by eosinophils. Benralizumab antibodies cover the eosinophil and induce natural killer cell-dependent cell death, depleting eosinophils. It reduces significant asthma exacerbations. Benralizumab is generally well-tolerated, but hypersensitivity reactions have been detected, including anaphylaxis, angioedema, and urticaria.
Dupilumab targets the IL‐4a receptor and blocks the signaling of both IL‐4 and IL‐13. It is used for patients with moderate to severe asthma, reducing asthma exacerbations by approximately 50% and significantly improving lung function within two weeks. Dupilumab has a successful safety profile, with side effects of injection site reaction and transient blood eosinophilia.
Mepolizumab and Reslizumab are monoclonal antibodies that bind to IL‐5, preventing it from binding to its receptor. They are used for patients with severe asthma and high blood eosinophils.
Definitions
AIT (Allergy Immunotherapy): a process that trains your body’s immune system to stop attacking harmless allergens so you don’t get allergic symptoms. It introduces small amounts of allergens into your body so your immune system can gradually learn to tolerate them
Anaphylaxis: an acute allergic reaction of the airways, in which the airway is normally constricted to extremely dangerous levels and can cause death
Biologics: any pharmaceutical drug manufactured with/in, extracted from, or semi-synthesized from biological sources, such as monoclonal antibodies
Ciliary beat frequency analysis: analyzing the frequency of the respiratory tract cilia beating that propels mucus towards the pharynx where it is swallowed
Nasal endoscopy: a procedure to look at the nasal and sinus passages done with an endoscope
Nasal smear cytology: a diagnostic tool in diagnosing nasal allergic disorders; allows clinicians to detect the changes of the nasal epithelium caused by exposure to physical or chemical, acute or chronic irritations.
Nasal cytology: a diagnostic procedure in which the normal and pathological aspects of the nasal mucosa are analyzed; involves identifying and counting the cell types and their morphology.Unilateral eosinophilia: a higher than normal level of eosinophils in one side of the nasal pathways or sinuses