An allergen is an antigen that one has an allergic reaction to from outside of the body that one breathes in, eats, or touches. Some examples of allergens that can be breathed/ taken in are foods, mold, pollen, dander, etc. There are two steps to an allergic reaction, sensitization (the first exposure) and subsequent exposure.
Sensitization
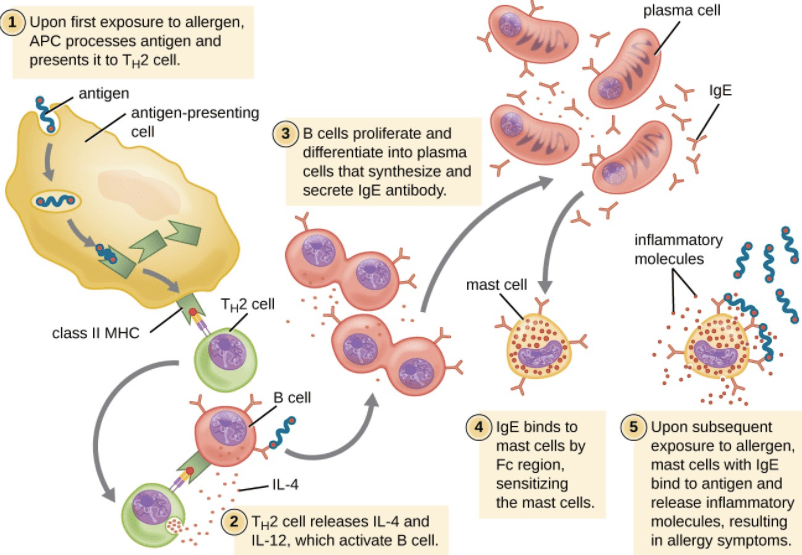
Sensitization may start with a person breathing in pollen, like ragweed pollen, for the first time. The allergen gets taken up by dendritic cells along the membranes of the airways. DCs process the allergen down into peptides (small sections of proteins) and present it on the outside of their cell membrane. The DC then migrates to the lymph nodes, where adaptive immune cells like T and B cells (see below) are mainly located. A naive T cell in the lymph node binds to the antigen and co-stimulatory molecules presented by the DC and differentiates into an activated helper T cell (Th cell).
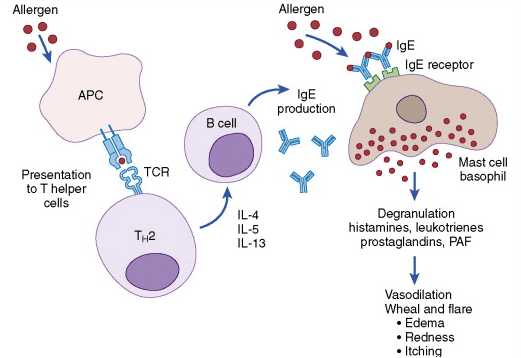
T-cells are immune cells (white blood cells) that are antigen-specific. T-cells are directed down an allergy-specific activation pathway by chemical messengers called cytokines released by innate immune cells around them. Activated helper T-cells can go on to activate B-cells (see below). T-cells can also identify and kill cells that have taken up an allergen. As most allergic reactions (including airway allergies) are a type I hypersensitivity, the T-cells differentiate into Th2 in response to cytokines in the local airway environment which include IL-4, IL-5, and IL-13. The activated Th2 cells can release more IL-4 to trigger B-cells to activate and initiate class switching to IgE (Immunoglobin E) antibodies. In addition, Th2 cells release IL-5 to increase production and activation of eosinophils. A subset of T and B-cells also mature into memory cells so that the body can recognize this allergen quicker with subsequent exposure. Antibodies against this allergen start circulating throughout the body and reach peak concentration around 10-14 days post-exposure.
Subsequent Exposure
When a person breathes in pollen again, IgE antibodies in circulation bind the pollen allergen and become cross-linked. Mast cells bind to the pollen allergen with its coat of antibodies, causing degranulation and release of allergic mediators. The effects of the cross-link are the “early phase reactions” and happen within minutes of the subsequent exposure.
The primary mediator released by mast cells is histamine. Histamines can take two pathways that affect the body. In the first pathway, histamine binds to H1 receptors which causes the smooth muscle pf the bronchi to contract and trigger difficulty breathing. Histamine also causes blood vessels to dilate, which increases the permeability of blood vessels and leads to edema, swelling, and mucous secretion (more in the airway).
There is then a late phase reaction which takes place eight to twelve hours after the subsequent exposure. This late phase reaction occurs because cytokines produced during the early phase cause more immune cells (helper T-cell 2, eosinophils, basophils) to migrate to the area with the allergen (IL-4, IL-5, and IL-10). Additionally, small molecules called leukotrienes damage the epithelium and attract immune cells even after the allergen is gone. Soon the symptoms will eventually die down as pro-inflammatory immune cells will no longer get signaled to go to the area where the allergen was.
Some of the mild symptoms of a type I hypersensitivity reaction are hives (urticaria), eczema, nose inflammation (allergic rhinitis), and asthma. Some of the more severe symptoms (usually caused by a large amount of an allergen) are increased vascular permeability and airway constriction, also known as anaphylactic shock.

Definitions:
Antibodies: A blood protein that counteracts a specific antigen. Antibodies combine chemically with substances that the body recognizes as foreign.
Basophils: Least common white blood cell type, made in bone marrow
Eosinophils: A type of infection-fighting white blood cell.
Granulocytes: a white blood cell that contains secretory granules (tiny sacs that contain various enzymes, compounds, and other components that are used to defend against pathogens, reduce inflammation and destroy cells) in its cytoplasm, i.e. a neutrophil, basophil, or eosinophil
Lymph node: Lymph nodes are glands that filter out the damaged cells. Lymph nodes filter substances that travel through the lymphatic fluid, and they contain lymphocytes (white blood cells) that help the body fight infection and disease
Mast cells: Allergy cells responsible for immediate allergic reactions. They cause allergic symptoms by releasing mediators stored inside of them or made by them
Mediator: compounds that are either locally released or carried in blood or tissue fluids and that help initiate, perpetuate, or aggravate a pathological process.
Type I Hypersensitivity: Include atopic diseases ( exaggerated IgE mediated immune responses (i.e., allergic: asthma, rhinitis, conjunctivitis, and dermatitis)), and allergic diseases(i.e., anaphylaxis, urticaria, angioedema, food, and drug allergies)